|
General info
a) What are haemorrhoids?
The word “haemorrhoids” is Greek for “blood flow”. A haemorrhoid is an anatomical region in the rectum consisting of arteriovenous vascular cushions in the rectal mucosa (distal rectal mucosa, corpus cavernosum recti). Everyone has haemorrhoids; they are part of the continence organ and therefore share responsibility for retaining faeces and bowel gas (“fine continence”). As soon as the rectum is full, the internal sphincter muscle tightens involuntarily. As it does so, some of the efferent blood vessels are constricted, the vascular cushion swells and so seals the anus. During defecation, the muscles relax, the blood is allowed to drain away, the swelling of the haemorrhoids goes down and defecation can take place unimpeded. A pathological state exists only if the vascular cushions are enlarged. Such vasodilation is usually seen in the region of the afferent arteries as nodular cushions (nodules) at 3, 7 and 11 o’clock in the “lithotomy position” (as for a gynaecological examination, where the patient lies on his back and places his legs in supports). Other smaller nodules (satellite nodules) may be present at 1, 5 and 9 o’clock. Enlargement of the haemorrhoidal cushions is not always noticed in the early stages and is not visible externally.
Only if the enlarged haemorrhoids cause anal discomfort do we talk of haemorrhoidal disease.
b) Anatomy
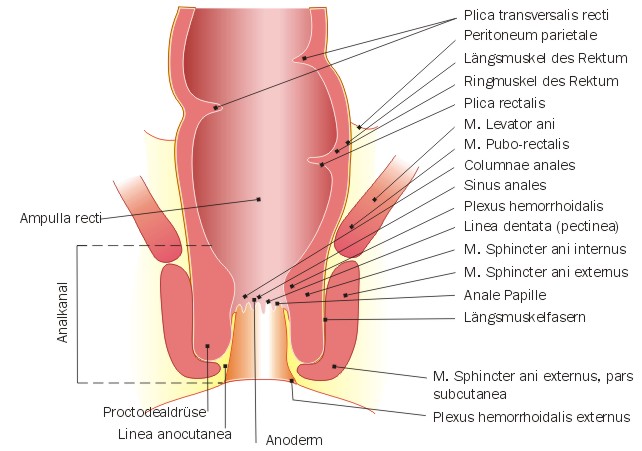 |
c) How common is haemorrhoidal disease?
Haemorrhoidal disease is a “lifestyle disease” that occurs mainly in Western industrialised nations, promoted by eating habits and a sedentary lifestyle and work regime. At least one in two people experience discomfort associated with their haemorrhoids once in their lifetime, as well as other accompanying anal disorders such as anal inflammation. The remaining tissue may often become enlarged again after treatment. Few data are available worldwide on the prevalence of haemorrhoidal disease.
d) Grading
Various nomenclatures are used, with a distinction often being made in the English-language nomenclature between “internal” and “external” haemorrhoids. While, on the one hand, externally prolapsing haemorrhoidal tissue can be described as “external” haemorrhoids, changes to the external perianal venous plexus are sometimes also mistakenly referred to as “external haemorrhoids”. These are generally acutely painful, usually multilocular thromboses in the perianal venous plexus (perianal thrombosis) or loose external skin flaps (skin tags) (see differential diagnoses). (Image)
Haemorrhoids are classified in 4 grades:
 |
 |
grade I: enlargement of the haemorrhoidal cushions, detectable only by means of rectal endoscopy (proctoscopy).
|
 |
 |
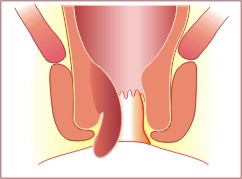
grade II: protrusion of the haemorrhoidal tissue (prolapse) out of the anal canal during defecation or when straining. At rest, the prolapsed haemorrhoidal nodules slip back into the anus (retraction) spontaneously.
|
 |
 |
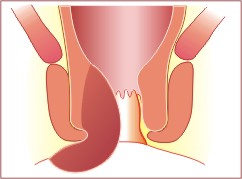
grade III: unlike grade II haemorrhoids, the protrusion of the haemorrhoidal tissue (prolapse), which may in this case occur even on walking for a while or on physical exertion, can only be reintroduced (reduced) manually.
|
 |
 |
grade IV: permanent protrusion of the haemorrhoidal tissue (prolapse), reintroduction (reduction) is impossible; in addition, usually, protrusion of the lining of the anal canal (anoderm), known as anal prolapse.
|
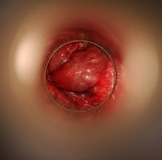
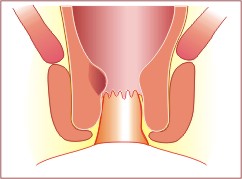
Haemorrhoids grade I
|
Hemorrhoidal node viewed by proctoscope
Enlarged hemorrhoids, they never prolapse and rarely produce symptomatology.
|

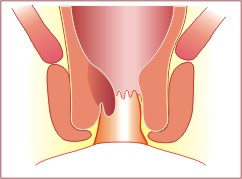
Haemorrhoids grade II
|
Prolapsed hemorrhoids while patient is pressing
Enlarged hemorrhoids can prolapse through the anal canal, but retract spontaneously.
|

Haemorrhoids grade III
|
Partial anal prolapse with traces of faeces
Hemorrhoids frequently prolapse, require manual replacement.
|

Haemorrhoids grade IV
|
With semi circular fixed anal prolapse
Permanently prolapsed.
|
e) What causes haemorrhoidal changes?
Overweight, eating the wrong foods, straining on defecation, childbirth or an inherited structural weakness may lead to enlargement and displacement of this vascular plexus, normally located above the sphincter muscles.
f) Risk factors
There is usually a combination of risk factors: - chronic constipation
- overuse of laxatives (laxative abuse) with loose stools
- women who have given birth several times suffer more commonly from haemorrhoids
- heavy lifting over a number of years
- inherited tendency (predisposition)
g) Psychosomatic aspects
Since the site of the disease is the anal region, initial presentation to a doctor is often delayed out of embarrassment. Pruritus (itching) in the anal region may in particular lead to psychosomatic problems that should not be underestimated.
|